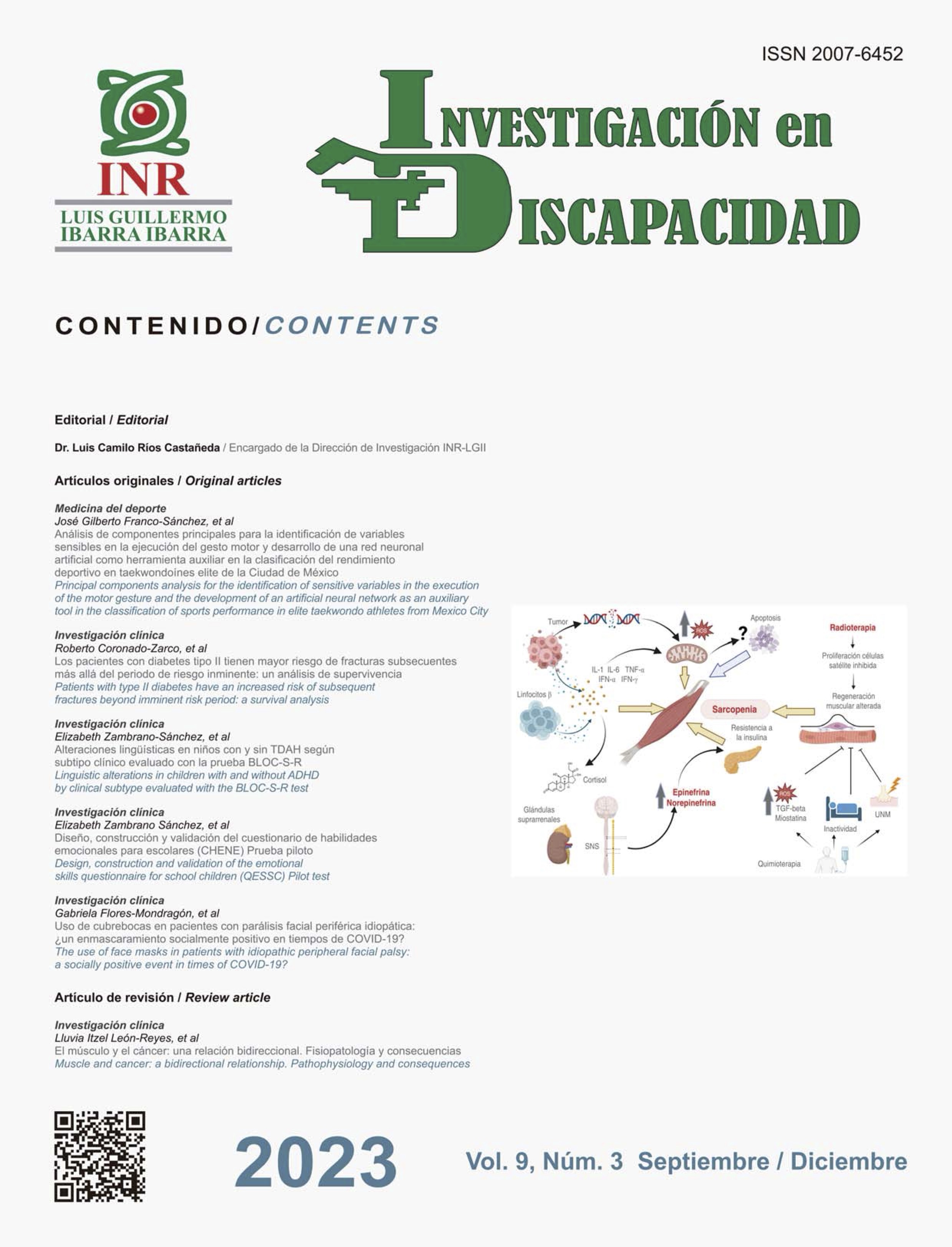
Muscle and cancer: a bidirectional relationship. Pathophysiology and consequences
DOI:
https://doi.org/10.35366/112699Keywords:
sarcopenia, cancer, mortality, survival, chemotherapy, radiotherapyAbstract
The muscle has very important interrelationships with other organs such as the heart, liver, brain and adipose tissue. Its wear, known as sarcopenia, has been associated with different types of cancer during treatment, which causes an increase in toxicity derived from both, chemotherapy and radiotherapy. This causes treatment delays and unwanted dose adjustments that negatively impact the survival of cancer patients. There is evidence that suggests that sarcopenia persists even in the survival stage, conditioning a negative impact on the quality of life of patients and on their work productivity. Different physiopathological mechanisms at the cellular and molecular level involved in sarcopenia in cancer are known, which increasingly show a bidirectional relationship, both positive and negative, between cancer and muscle.
Publication Facts
Reviewer profiles N/A
Author statements
Indexed in
- Academic society
- N/A
References
Lee JH, Jun HS. Role of myokines in regulating skeletal
muscle mass and function. Front Physiol. 2019; 10: 42.
Available in: https://doi.org/10.3389/fphys.2019.00042
Chen W, Wang L, You W, Shan T. Myokines mediate
the cross talk between skeletal muscle and other organs.
J Cell Physiol. 2021; 236 (4): 2393-2412. Available in:
https://doi.org/10.1002/jcp.30033
Peixoto da Silva S, Santos JMO, Costa ESMP, Gil
da Costa RM, Medeiros R. Cancer cachexia and its
pathophysiology: links with sarcopenia, anorexia and
asthenia. J Cachexia Sarcopenia Muscle. 2020; 11
(3): 619-635. Available in: https://doi.org/10.1002/
jcsm.12528
Ryan AM, Power DG, Daly L, Cushen SJ, Ni Bhuachalla
E, Prado CM. Cancer-associated malnutrition, cachexia
and sarcopenia: the skeleton in the hospital closet 40
years later. Proc Nutr Soc. 2016; 75 (2): 199-211. Available
in: https://doi.org/10.1017/S002966511500419X
Ness KK, Hudson MM, Pui CH, Green DM, Krull
KR, Huang TT et al. Neuromuscular impairments
in adult survivors of childhood acute lymphoblastic
leukemia: associations with physical performance and
chemotherapy doses. Cancer. 2012; 118 (3): 828-838.
Available in: https://doi.org/10.1002/cncr.26337
Khal J, Wyke SM, Russell ST, Hine AV, Tisdale MJ.
Expression of the ubiquitin-proteasome pathway and
muscle loss in experimental cancer cachexia. Br J
Cancer. 2005; 93 (7): 774-780. Available in: https://doi.
org/10.1038/sj.bjc.6602780
White JP, Baynes JW, Welle SL, Kostek MC, Matesic LE,
Sato S et al. The regulation of skeletal muscle protein
turnover during the progression of cancer cachexia in
the Apc(Min/+) mouse. PLoS One. 2011; 6 (9): e24650.
https://doi.org/10.1371/journal.pone.0024650
Hartman A, Van den Bos C, Stijnen T, Pieters R.
Decrease in peripheral muscle strength and ankle
dorsiflexion as long-term side effects of treatment
for childhood cancer. Pediatr Blood Cancer. 2008;
(4): 833-837. Available in: https://doi.org/10.1002/
pbc.21325
Global Burden of Disease Cancer C, Kocarnik JM,
Compton K, Dean FE, Fu W, Gaw BL et al. Cancer
Incidence, Mortality, Years of Life Lost, Years Lived
With Disability, and Disability-Adjusted Life Years for
Cancer Groups From 2010 to 2019: A Systematic
Analysis for the Global Burden of Disease Study 2019.
JAMA Oncol. 2022; 8 (3): 420-444.
Bauer J, Morley JE, Schols A, Ferrucci L, Cruz-Jentoft
AJ, Dent E et al. Sarcopenia: a time for action. An SCWD
position paper. J Cachexia Sarcopenia Muscle. 2019;
(5): 956-961. Available in: https://doi.org/10.1002/
jcsm.12483
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere
O, Cederholm T, Cooper C et al. Sarcopenia: revised
European consensus on definition and diagnosis. Age
Ageing. 2019; 48 (4): 601. Available in: https://doi.
org/10.1093/ageing/afz046
Xu J, Wan CS, Ktoris K, Reijnierse EM, Maier AB.
Sarcopenia Is Associated with Mortality in Adults: A
Systematic Review and Meta-Analysis. Gerontology.
; 68 (4): 361-376. Available in: https://doi.
org/10.1159/000517099
Ritz A, Lurz E, Berger M. Sarcopenia in children with
solid organ tumors: an instrumental era. Cells. 2022;
(8): 1278. Available in: https://doi.org/10.3390/
cells11081278
Ormsbee MJ, Prado CM, Ilich JZ, Purcell S, Siervo M,
Folsom A, Panton L. Osteosarcopenic obesity: the role of
bone, muscle, and fat on health. J Cachexia Sarcopenia
Muscle. 2014; 5 (3): 183-192. Available in: https://doi.
org/10.1007/s13539-014-0146-x
Waters DL, Baumgartner RN. Sarcopenia and obesity.
Clin Geriatr Med. 2011; 27 (3): 401-421. Available in:
https://doi.org/10.1016/j.cger.2011.03.007
Villasenor A, Ballard-Barbash R, Baumgartner K,
Baumgartner R, Bernstein L, McTiernan A et al.
Prevalence and prognostic effect of sarcopenia in
breast cancer survivors: the HEAL Study. J Cancer
Surviv. 2012; 6 (4): 398-406. Available in: https://doi.
org/10.1007/s11764-012-0234-x
Williams AM, Krull KR, Howell CR, Banerjee P,
Brinkman TM, Kaste SC et al. Physiologic frailty and
neurocognitive decline among young-adult childhood
cancer survivors: a prospective study from the St
Jude Lifetime cohort. J Clin Oncol, 2021; 39 (31):
-3495. Available in: https://doi.org/10.1200/
JCO.21.00194
Tomlinson D, Zupanec S, Jones H, O’Sullivan C, Hesser
T, Sung L. The lived experience of fatigue in children and
adolescents with cancer: a systematic review. Support
Care Cancer. 2016; 24 (8): 3623-3631. Available in:
https://doi.org/10.1007/s00520-016-3253-8
Prado CM, Baracos VE, McCargar LJ, Reiman
T, Mourtzakis M, Tonkin K et al. Sarcopenia as a
determinant of chemotherapy toxicity and time to
tumor progression in metastatic breast cancer patients
receiving capecitabine treatment. Clin Cancer Res.
; 15 (8): 2920-2926. Available in: https://doi.
org/10.1158/1078-0432.CCR-08-2242
Cao A, Ferrucci LM, Caan BJ, Irwin ML. Effect of
exercise on sarcopenia among cancer survivors: a
systematic review. Cancers (Basel). 2022; 14 (3).
Available in: https://doi.org/10.3390/cancers14030786
Prado CM, Cushen SJ, Orsso CE, Ryan AM. Sarcopenia
and cachexia in the era of obesity: clinical and nutritional
impact. Proc Nutr Soc. 2016; 75 (2): 188-198. Available
in: https://doi.org/10.1017/S0029665115004279
Brown JL, Lee DE, Rosa-Caldwell ME, Brown LA,
Perry RA, Haynie WS et al. Protein imbalance in the
development of skeletal muscle wasting in tumour-bearing
mice. J Cachexia Sarcopenia Muscle. 2018; 9 (5): 987-
Available in: https://doi.org/10.1002/jcsm.12354
Bechet D, Tassa A, Taillandier D, Combaret L, Attaix D.
Lysosomal proteolysis in skeletal muscle. Int J Biochem
Cell Biol. 2005; 37 (10): 2098-2114. Available in: https://
doi.org/10.1016/j.biocel.2005.02.029
Glick D, Barth S, Macleod KF. Autophagy: cellular and
molecular mechanisms. J Pathol. 2010; 221 (1): 3-12.
Available in: https://doi.org/10.1002/path.2697
Pettersen K, Andersen S, Degen S, Tadini V, Grosjean
J, Hatakeyama S et al. Cancer cachexia associates
with a systemic autophagy-inducing activity mimicked
by cancer cell-derived IL-6 trans-signaling. Sci Rep.
; 7 (1): 2046. Available in: https://doi.org/10.1038/
s41598-017-02088-2
Kraft CS, LeMoine CM, Lyons CN, Michaud D, Mueller
CR, Moyes CD. Control of mitochondrial biogenesis
during myogenesis. Am J Physiol Cell Physiol. 2006; 290
(4): C1119-1127. Available in: https://doi.org/10.1152/
ajpcell.00463.2005
Mallard J, Hucteau E, Charles AL, Bender L, Baeza
C, Pelissie M et al. Chemotherapy impairs skeletal
muscle mitochondrial homeostasis in early breast
cancer patients. J Cachexia Sarcopenia Muscle. 2022;
(3): 1896-1907. Available in: https://doi.org/10.1002/
jcsm.12991
Berg HE, Eiken O, Miklavcic L, Mekjavic IB. Hip, thigh
and calf muscle atrophy and bone loss after 5-week
bedrest inactivity. Eur J Appl Physiol. 2007; 99 (3):
-289. Available in: https://doi.org/10.1007/s00421-
-0346-y
Evans WJ. Skeletal muscle loss: cachexia, sarcopenia,
and inactivity. Am J Clin Nutr. 2010; 91 (4): 1123S-1127S.
Available in: https://doi.org/10.3945/ajcn.2010.28608A
Costelli P, Muscaritoli M, Bossola M, Penna F, Reffo P,
Bonetto A et al. IGF-1 is downregulated in experimental
cancer cachexia. Am J Physiol Regul Integr Comp
Physiol. 2006; 291 (3): R674-683. Available in: https://
doi.org/10.1152/ajpregu.00104.2006
Dirks-Naylor AJ, Griffiths CL. Glucocorticoid-induced
apoptosis and cellular mechanisms of myopathy. J
Steroid Biochem Mol Biol. 2009; 117 (1-3): 1-7. Available
in: https://doi.org/10.1016/j.jsbmb.2009.05.014
Sambasivan R, Tajbakhsh S. Adult skeletal muscle
stem cells. Results Probl Cell Differ. 2015; 56: 191-213.
Available in: https://doi.org/10.1007/978-3-662-44608-
_9
Michele DE. Mechanisms of skeletal muscle repair and
regeneration in health and disease. FEBS J. 2022; 289
(21): 6460-6462. Available in: https://doi.org/10.1111/
febs.16577
Bentzinger CF, Wang YX, Dumont NA, Rudnicki MA.
Cellular dynamics in the muscle satellite cell niche.
EMBO Rep. 2013; 14 (12): 1062-1072. Available in:
https://doi.org/10.1038/embor.2013.182
Tedesco FS, Dellavalle A, Diaz-Manera J, Messina
G, Cossu G. Repairing skeletal muscle: regenerative
potential of skeletal muscle stem cells. J Clin Invest.
; 120 (1): 11-19. https://doi.org/10.1172/JCI40373
Kim J, Lee J. Role of transforming growth factor-beta
in muscle damage and regeneration: focused on
eccentric muscle contraction. J Exerc Rehabil. 2017;
(6): 621-626. Available in: https://doi.org/10.12965/
jer.1735072.536
Ballinger TJ, Thompson WR, Guise TA. The bone-
muscle connection in breast cancer: implications and
therapeutic strategies to preserve musculoskeletal
health. Breast Cancer Res. 2022; 24 (1): 84. Available
in: https://doi.org/10.1186/s13058-022-01576-2
Davis MP, Panikkar R. Sarcopenia associated with
chemotherapy and targeted agents for cancer therapy.
Ann Palliat Med. 2019; 8 (1): 86-101. Available in: https://
doi.org/10.21037/apm.2018.08.02
Marques VA, Ferreira-Junior JB, Lemos TV, Moraes RF,
Junior JRS, Alves RR et al. Effects of chemotherapy
treatment on muscle strength, quality of life, fatigue, and
anxiety in women with breast cancer. Int J Environ Res
Public Health. 2020; 17 (19): 7289. Available in: https://
doi.org/10.3390/ijerph17197289
Braun TP, Szumowski M, Levasseur PR, Grossberg
AJ, Zhu X, Agarwal A et al. Muscle atrophy in response
to cytotoxic chemotherapy is dependent on intact
glucocorticoid signaling in skeletal muscle. PLoS
One. 2014; 9 (9): e106489. Available in: https://doi.
org/10.1371/journal.pone.0106489
Damrauer JS, Stadler ME, Acharyya S, Baldwin AS,
Couch ME, Guttridge DC. Chemotherapy-induced
muscle wasting: association with NF-kappaB and
cancer cachexia. Eur J Transl Myol. 2018; 28 (2): 7590.
Available in: https://doi.org/10.4081/ejtm.2018.7590
Barreto R, Waning DL, Gao H, Liu Y, Zimmers
TA, Bonetto A. Chemotherapy-related cachexia is
associated with mitochondrial depletion and the
activation of ERK1/2 and p38 MAPKs. Oncotarget,
; 7 (28): 43442-43460. Available in: https://doi.
org/10.18632/oncotarget.9779
Chen JL, Colgan TD, Walton KL, Gregorevic P, Harrison
CA. The TGF-beta Signalling Network in Muscle
Development, Adaptation and Disease. Adv Exp Med
Biol. 2016; 900: 97-131. https://doi.org/10.1007/978-3-
-27511-6_5
Yu Y, Feng XH. TGF-beta signaling in cell fate control
and cancer. Curr Opin Cell Biol. 2019; 61: 56-63.
Available in: https://doi.org/10.1016/j.ceb.2019.07.007
Huang L, Li W, Lu Y, Ju Q, Ouyang M. Iron metabolism
in colorectal cancer. Front Oncol. 2023; 13: 1098501.
Available in: https://doi.org/10.3389/fonc.2023.1098501
Okazaki Y, Hino K. Iron and cancer: a special issue.
Cancers (Basel). 2023; 15 (7): Available in: https://doi.
org/10.3390/cancers15072097
Wyart E, Hsu MY, Sartori R, Mina E, Rausch V, Pierobon
ES et al. Iron supplementation is sufficient to rescue
skeletal muscle mass and function in cancer cachexia.
EMBO Rep. 2022; 23 (4): e53746. Available in: https://
doi.org/10.15252/embr.202153746
Arpke RW, Shams AS, Collins BC, Larson AA, Lu N,
Lowe DA et al. Preservation of satellite cell number
and regenerative potential with age reveals locomotory
muscle bias. Skelet Muscle. 2021; 11 (1): 22. Available
in: https://doi.org/10.1186/s13395-021-00277-2
Fukada SI, Higashimoto T, Kaneshige A. Differences
in muscle satellite cell dynamics during muscle
hypertrophy and regeneration. Skelet Muscle. 2022; 12
(1): 17. Available in: https://doi.org/10.1186/s13395-022-
-0
Dumont NA, Bentzinger CF, Sincennes MC, Rudnicki
MA. Satellite cells and skeletal muscle regeneration.
Compr Physiol. 2015; 5 (3): 1027-1059. Available in:
https://doi.org/10.1002/cphy.c140068
Zeng X, Xie L, Ge Y, Zhou Y, Wang H, Chen Y, et al.
Satellite cells are activated in a rat model of radiation-
induced muscle fibrosis. Radiat Res. 2022; 197 (6):
-649. Available in: https://doi.org/10.1667/RADE-
-00183.1
Caiozzo VJ, Giedzinski E, Baker M, Suarez T, Izadi A,
Lan M, et al. The radiosensitivity of satellite cells: cell
cycle regulation, apoptosis and oxidative stress. Radiat
Res. 2010; 174 (5): 582-589. Available in: https://doi.
org/10.1667/RR2190.1
Paulino AC, Wen BC, Brown CK, Tannous R, Mayr
NA, Zhen WK et al. Late effects in children treated with
radiation therapy for Wilms’ tumor. Int J Radiat Oncol
Biol Phys. 2000; 46 (5): 1239-1246. Available in: https://
doi.org/10.1016/s0360-3016(99)00534-9
D’Souza D, Roubos S, Larkin J, Lloyd J, Emmons
R, Chen H et al. The late effects of radiation therapy
on skeletal muscle morphology and progenitor cell
content are influenced by diet-induced obesity and
exercise training in male mice. Sci Rep. 2019; 9 (1):
Available in: https://doi.org/10.1038/s41598-019-
-8
Jung HW, Kim JW, Kim JY, Kim SW, Yang HK, Lee
JW et al. Effect of muscle mass on toxicity and survival
in patients with colon cancer undergoing adjuvant
chemotherapy. Support Care Cancer. 2015; 23 (3):
-694. Available in: https://doi.org/10.1007/s00520-
-2418-6
Schakman O, Gilson H, Thissen JP. Mechanisms of
glucocorticoid-induced myopathy. J Endocrinol. 2008;
(1): 1-10. Available in: https://doi.org/10.1677/JOE-
-0606
Chapman MA, Meza R, Lieber RL. Skeletal muscle
fibroblasts in health and disease. Differentiation. 2016;
(3): 108-115. Available in: https://doi.org/10.1016/j.
diff.2016.05.007
Case AA, Kullgren J, Anwar S, Pedraza S, Davis
MP. Treating chronic pain with buprenorphine-the
practical guide. Curr Treat Options Oncol. 2021; 22
(12): 116. Available in: https://doi-org.pbidi.unam.
mx:2443/10.1007/s11864-021-00910-8
Lin T, Dai M, Xu P, Sun L, Shu X, Xia X et al. Prevalence
of sarcopenia in pain patients and correlation between
the two conditions: a systematic review and meta-
analysis. J Am Med Dir Assoc. 2022; 23 (5): 902.
e1-902.e20. Available in: https://doi-org.pbidi.unam.
mx:2443/10.1016/j.jamda.2022.02.005
Mucke M, Weier M, Carter C, Copeland J, Degenhardt
L, Cuhls H et al. Systematic review and meta-analysis
of cannabinoids in palliative medicine. J Cachexia
Sarcopenia Muscle. 2018; 9 (2): 220-234. Available in:
https://doi-org.pbidi.unam.mx:2443/10.1002/jcsm.12273
Schouten M, Dalle S, Koppo K. Molecular Mechanisms
Through Which Cannabidiol May Affect Skeletal Muscle
Metabolism, Inflammation, Tissue Regeneration, and
Anabolism: A Narrative Review. Cannabis Cannabinoid
Res. 2022; 7(6): 745-757.
Overholser LS, Callaway C. Preventive health in cancer
survivors: what should we be recommending? J Natl
Compr Canc Netw. 2018; 16 (10): 1251-1258. Available
in: https://doi.org/10.6004/jnccn.2018.7083
Pérez CDA, Allende PSR, Verastegui AE, Rivera
FMM, Meneses GA, Herrera GA et al. Assessment
and impact of phase angle and sarcopenia in palliative
cancer patients. Nutr Cancer. 2017; 69 (8): 1227-1233.
Available in: https://doi-org.pbidi.unam.mx:2443/10.108
/01635581.2017.1367939
Ruiz-Casado A, Alvarez-Bustos A, de Pedro CG,
Mendez-Otero M, Romero-Elias M. Cancer-related
fatigue in breast cancer survivors: a review. Clin Breast
Cancer. 2021; 21 (1): 10-25. Available in: https://doi.
org/10.1016/j.clbc.2020.07.011
Van Deuren S, Boonstra A, Van Dulmen-den Broeder
E, Blijlevens N, Knoop H, Loonen J. Severe fatigue after
treatment for childhood cancer. Cochrane Database
Syst Rev. 2020; 3: CD012681. Available in: https://doi.
org/10.1002/14651858.CD012681.pub2
Lee SJ, Park YJ, Cartmell KB. Sarcopenia in cancer
survivors is associated with increased cardiovascular
disease risk. Support Care Cancer. 2018; 26 (7): 2313-
Available in: https://doi.org/10.1007/s00520-018-
-7
Goodenough CG, Partin RE, Ness KK. Skeletal muscle
and childhood cancer: where are we now and where
we go from here. Aging Cancer. 2021; 2 (1-2): 13-35.
Available in: https://doi.org/10.1002/aac2.12027
Hockenberry-Eaton M, Hinds PS. Fatigue in children
and adolescents with cancer: evolution of a program
of study. Semin Oncol Nurs. 2000; 16 (4): 261-
; discussion 272-268. Available in: https://doi.
org/10.1053/sonu.2000.16577
Van Dijk-Lokkart EM, Steur LMH, Braam KI, Veening
MA, Huisman J, Takken T et al. Longitudinal
development of cancer-related fatigue and physical
activity in childhood cancer patients. Pediatr Blood
Cancer. 2019; 66 (12): e27949. Available in: https://
doi.org/10.1002/pbc.27949
Paulino AC. Late effects of radiotherapy for pediatric
extremity sarcomas. Int J Radiat Oncol Biol Phys. 2004;
(1): 265-274. Available in: https://doi.org/10.1016/j.
ijrobp.2004.02.001
Stokes CL, Stokes WA, Kalapurakal JA, Paulino AC,
Cost NG, Cost CR et al. Timing of radiation therapy
in pediatric Wilms tumor: a report from the national
cancer database. Int J Radiat Oncol Biol Phys. 2018;
(2): 453-461. Available in: https://doi.org/10.1016/j.
ijrobp.2018.01.110
Hetzler KL, Hardee JP, Puppa MJ, Narsale AA, Sato
S, Davis JM et al. Sex differences in the relationship of
IL-6 signaling to cancer cachexia progression. Biochim
Biophys Acta. 2015; 1852 (5): 816-825. Available in:
https://doi.org/10.1016/j.bbadis.2014.12.015
Hetzler KL, Hardee JP, LaVoie HA, Murphy EA, Carson
JA. Ovarian function’s role during cancer cachexia
progression in the female mouse. Am J Physiol
Endocrinol Metab. 2017; 312 (5): E447-E459. Available
in: https://doi.org/10.1152/ajpendo.00294.2016
Wang X, Pickrell AM, Zimmers TA, Moraes CT. Increase
in muscle mitochondrial biogenesis does not prevent
muscle loss but increased tumor size in a mouse model
of acute cancer-induced cachexia. PLoS One. 2012; 7
(3): e33426. Available in: https://doi.org/10.1371/journal.
pone.0033426
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Instituto Nacional de Rehabilitación Luis Guillermo Ibarra Ibarra

This work is licensed under a Creative Commons Attribution 4.0 International License.
© Instituto Nacional de Rehabilitación Luis Guillermo Ibarra Ibarra under a Creative Commons Attribution 4.0 International (CC BY 4.0) license which allows to reproduce and modify the content if appropiate recognition to the original source is given.