Lesiones de manguito rotador: estado actual de la literatura con enfoque en rehabilitación
DOI:
https://doi.org/10.35366/109508Palabras clave:
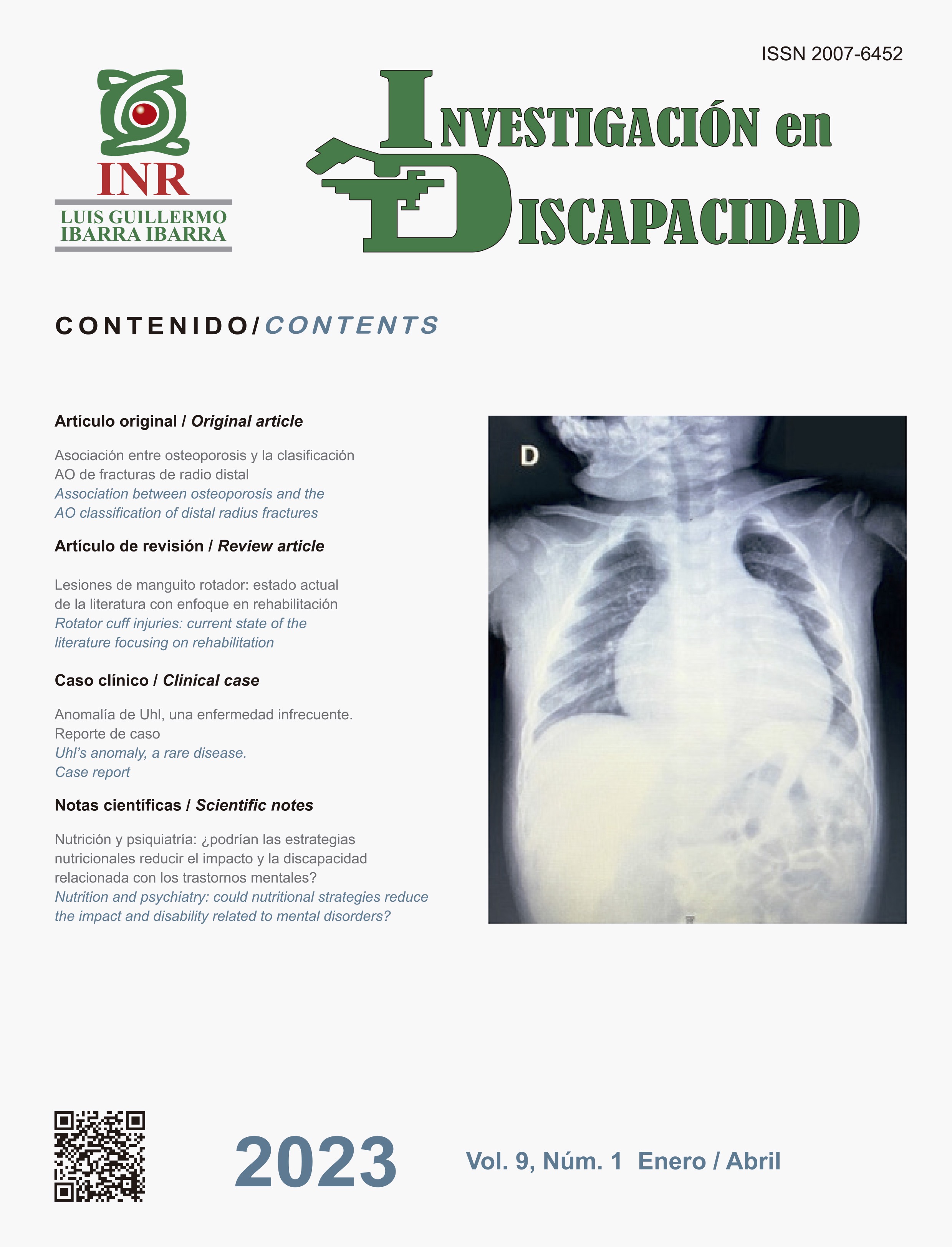
hombro doloroso, lesiones del manguito rotador, diagnóstico, terapéutica, rehabilitaciónResumen
Las lesiones de manguito rotador son la principal causa de hombro doloroso. La evidencia y recomendaciones sobre su diagnóstico, tratamiento y rehabilitación se actualizan con rapidez. Clínicamente, se caracterizan por dolor localizado en hombro, cuello, brazo y región escapular, además de debilidad y limitación funcional. Es necesario realizar una evaluación clínica adecuada para tener un diagnóstico certero, así como llevar a cabo estudios complementarios. El tratamiento inicial es conservador y consiste en la combinación de medicamentos, fisioterapia y recomendaciones de cuidados articulares. La rehabilitación es básica en el tratamiento conservador, pre y postquirúrgico. El ejercicio es la intervención más eficaz en el tratamiento y la piedra angular de la rehabilitación. Conocer las bases del diagnóstico y tratamiento inicial permite al clínico elaborar programas basados en el paciente y su reintegración funcional. Este artículo de revisión profundiza en los puntos anteriores, al brindar una perspectiva general de las lesiones del manguito rotador y su proceso de rehabilitación.
##plugins.generic.pfl.publicationFactsTitle##
##plugins.generic.pfl.reviewerProfiles## N/D
##plugins.generic.pfl.authorStatements##
Indexado: {$indexList}
-
##plugins.generic.pfl.indexedList##
- ##plugins.generic.pfl.academicSociety##
- N/D
Citas
Snedeker JG, Foolen J. Tendon injury and repair - A
perspective on the basic mechanisms of tendon disease
and future clinical therapy. Acta Biomater. 2017; 63:
-36. doi: 10.1016/j.actbio.2017.08.032.
Ackermann PW, Renström P. Tendinopathy in
sport. Sports Health. 2012; 4 (3): 193-201. doi:
1177/1941738112440957.
HodgettsC, Walker B. Epidemiology, common
diagnoses, treatments and prognosis of shoulder pain:
a narrative review. International Journal of Osteopathic
Medicine 2021; 42: 11-19.doi: https://doi.org/10.1016/j.
ijosm.2021.10.006.
Gombera MM, Sekiya JK. Rotator cuff tear and
glenohumeral instability: a systematic review. Clin
Orthop Relat Res. 2014; 472 (8): 2448-2456. doi:
1007/s11999-013-3290-2. Erratum in: Clin Orthop
Relat Res. 2015 Feb;473(2):751. Gomberawalla, M
Mustafa [correctedtoGombera, MufaddalMustafa].
Whittle S, Buchbinder R. In the clinic. Rotator cuff
disease. Ann Intern Med. 2015; 162 (1): ITC1-15. doi:
7326/AITC201501060.
Keough N, Lorke DE. The humeral head: a review of the
blood supply and possible link to osteonecrosis following
rotator cuff repair. J Anat. 2021; 239 (5): 973-982. doi:
1111/joa.13496.
Verhaegen F, Meynen A, Matthews H, Claes P,
Debeer P, Scheys L. Determination of pre-arthropathy
scapular anatomy with a statistical shape model:
part I-rotator cuff tear arthropathy. J Shoulder Elbow
Surg. 2021; 30 (5): 1095-1106. doi: 10.1016/j.
jse.2020.07.043.
Teunis T, Lubberts B, Reilly BT, Ring D. A systematic
review and pooled analysis of the prevalence of rotator
cuff disease with increasing age. J Shoulder Elbow Surg.
; 23 (12): 1913-1921. doi: 10.1016/j.jse.2014.08.001.
Yamaguchi K, Ditsios K, Middleton WD, Hildebolt
CF, Galatz LM, Teefey SA. The demographic and
morphological features of rotator cuff disease. A
comparison of asymptomatic and symptomatic
shoulders. J Bone Joint Surg Am. 2006; 88 (8): 1699-
doi: 10.2106/JBJS.E.00835.
Tempelhof S, Rupp S, Seil R. Age-related prevalence of
rotator cuff tears in asymptomatic shoulders. J Shoulder
Elbow Surg. 1999; 8 (4): 296-299. doi: 10.1016/s1058-
(99)90148-9.
Yamamoto A, Takagishi K, Kobayashi T, Shitara H,
Ichinose T, Takasawa E, Shimoyama D, Osawa T. The
impact of faulty posture on rotator cuff tears with and
without symptoms. J Shoulder Elbow Surg. 2015; 24
(3): 446-452. doi: 10.1016/j.jse.2014.07.012.
Reilly P, Macleod I, Macfarlane R, Windley J, Emery
RJ. Dead men and radiologists don’t lie: a review of
cadaveric and radiological studies of rotator cuff tear
prevalence. Ann R Coll Surg Engl. 2006; 88 (2): 116-
doi: 10.1308/003588406X94968.
Nho SJ, Yadav H, Shindle MK, Macgillivray JD.
Rotator cuff degeneration: etiology and pathogenesis.
Am J Sports Med. 2008; 36 (5): 987-993. doi:
1177/0363546508317344.
Bishop JY, Santiago-Torres JE, Rimmke N, Flanigan
DC. Smoking predisposes to rotator cuff pathology
and shoulder dysfunction: a systematic review.
Arthroscopy. 2015; 31 (8): 1598-605. doi: 10.1016/j.
arthro.2015.01.026.
Baumgarten KM, Gerlach D, Galatz LM, Teefey SA,
Middleton WD, Ditsios K, Yamaguchi K. Cigarette
smoking increases the risk for rotator cuff tears. Clin
OrthopRelat Res. 2010; 468 (6): 1534-1541. doi:
1007/s11999-009-0781-2.
Weber S, Chahal J. Management of rotator cuff injuries.
J Am Acad Orthop Surg. 2020; 28 (5): e193-e201. doi:
5435/JAAOS-D-19-00463.
Walker-Bone K, van der Windt DA. Shoulder pain -
where are we now? Curr Treat Options in Rheum.
;7: 285-306. doi:10.1007/s40674-021-00184-z.
Yoon TH, Choi CH, Kim SJ, Choi YR, Yoon SP, Chun
YM. Attrition of rotator cuff without progression to
tears during 2-5 years of conservative treatment for
impingement syndrome. ArchOrthop Trauma Surg.
; 139 (3): 377-382. doi: 10.1007/s00402-018-
-z.
Ueda Y, Sugaya H, Takahashi N, et al. Rotator cuff
lesions in patients with stiff shoulders: a prospective
analysis of 379 shoulders. J Bone Joint Surg Am. 2015;
(15): 1233-1237. doi: 10.2106/JBJS.N.00910.
Lewis J. Rotator cuff related shoulder pain: assessment,
management and uncertainties. Man Ther. 2016; 23:
-68. doi: 10.1016/j.math.2016.03.009.
White JJ, Titchener AG, Fakis A, Tambe AA, Hubbard
RB, Clark DI. An epidemiological study of rotator cuff
pathology using The Health Improvement Network
database. Bone Joint J. 2014; 96-B (3): 350-353. doi:
1302/0301-620X.96B3.32336.
Hermans J, Luime JJ, Meuffels DE, Reijman M, Simel
DL, Bierma-Zeinstra SM. Does this patient with shoulder
pain have rotator cuff disease?: The Rational Clinical
Examination systematic review. JAMA. 2013; 310 (8):
-847. doi: 10.1001/jama.2013.276187.
Hanchard NC, Lenza M, Handoll HH, Takwoingi Y.
Physical tests for shoulder impingements and local
lesions of bursa, tendon or labrum that may accompany
impingement. Cochrane Database Syst Rev. 2013; 2013
(4): CD007427. doi: 10.1002/14651858.CD007427.
pub2.
Hanchard NC, Howe TE, Gilbert MM. Diagnosis of
shoulder pain by history and selective tissue tension:
agreement between assessors. J Orthop Sports
Phys Ther. 2005; 35 (3): 147-153. doi: 10.2519/
jospt.2005.35.3.147.
Weber S, Chahal J. Case Studies AAOS Clinical Practice
Guideline: Management of Rotator Cuff Injuries. J
Am Acad Orthop Surg. 2021; 29 (3): e104-e108. doi:
5435/JAAOS-D-20-00450.
Park HB, Yokota A, Gill HS et al. Diagnostic accuracy
of clinical tests for the different degrees of subacromial
impingement syndrome. J Bone Joint Surg Am. 2005;
: 1446-1455.
Hertel R, Ballmer FT, Lombert SM et al. Lag signs in
the diagnosis of rotator cuff rupture. J Shoulder Elbow
Surg. 1996; 5: 307-313.
Gerber C, Krushell RJ. Isolated rupture of the tendon
of the subscapularis muscle. Clinical features in 16
cases. J Bone Joint Surg Br. 1991; 73 (3): 389-394. doi:
1302/0301-620X.73B3.1670434.
Jobe FW, Kvitne RS, Giangarra CE. Shoulder pain in
the overhand or throwing athlete. The relationship of
anterior instability and rotator cuff impingement. Orthop
Rev. 1989; 18 (9): 963-975. Erratum in: Orthop Rev.
; 18 (12): 1268. Giangarra, C E [added].
Leroux JL, Thomas E, Bonnel F, Blotman F. Diagnostic
value of clinical tests for shoulder impingement
syndrome. Rev Rhum Engl Ed. 1995; 62 (6): 423-428.
Barth JR, Burkhart SS, De Beer JF. The bear-hug test:
a new and sensitive test for diagnosing a subscapularis
tear. Arthroscopy. 2006; 22 (10): 1076-1084. doi:
1016/j.arthro.2006.05.005.
Maman E, Harris C, White L, Tomlinson G, Shashank
M, Boynton E. Outcome of nonoperative treatment of
symptomatic rotator cuff tears monitored by magnetic
resonance imaging. J Bone Joint Surg Am. 2009; 91
(8): 1898-1906. doi: 10.2106/JBJS.G.01335.
Petersson CJ, Redlund-Johnell I. The subacromial space
in normal shoulder radiographs. Acta Orthop Scand.
; 55 (1): 57-58. doi: 10.3109/17453678408992312.
Bartoszewski N, Parnes N. Rotator cuff injuries.
JAAPA. 2018; 31 (4): 49-50. doi: 10.1097/01.
JAA.0000531046.74384.c7.
Itoi E, Minagawa H, Yamamoto N, Seki N, Abe H. Are
pain location and physical examinations useful in locating
a tear site of the rotator cuff? Am J Sports Med. 2006;
(2): 256-264. doi: 10.1177/0363546505280430.
Kijima H, Minagawa H, Yamamoto N, et al. Three-
dimensional ultrasonography of shoulders with rotator
cuff tears. J Orthop Sci. 2008; 13 (6): 510-513. doi:
1007/s00776-008-1268-9.
Lee JC, Guy S, Connell D, Saifuddin A, Lambert S. MRI
of the rotator interval of the shoulder. Clin Radiol. 2007;
(5): 416-423. doi: 10.1016/j.crad.2006.11.017.
Smith TO, Back T, Toms AP, Hing CB. Diagnostic
accuracy of ultrasound for rotator cuff tears in adults: a
systematic review and meta-analysis. Clin Radiol. 2011;
(11): 1036-1048. doi: 10.1016/j.crad.2011.05.007.
Okoroha KR, Fidai MS, Tramer JS, Davis KD, Kolowich
PA. Diagnostic accuracy of ultrasound for rotator cuff
tears. Ultrasonography. 2019; 38 (3): 215-220. doi:
14366/usg.18058.
McCrum E. MR Imaging of the rotator cuff. Magn Reson
Imaging Clin N Am. 2020; 28 (2): 165-179. doi: 10.1016/j.
mric.2019.12.002.
Ryosa A, Laimi K, Aarimaa V, Lehtimaki K, Kukkonen J,
Saltychev M. Surgery or conservative treatment for rotator
cuff tear: a meta-analysis. Disabil Rehabil. 2017; 39 (14):
-1363. doi: 10.1080/09638288.2016.1198431.
Doiron-Cadrin P, Lafrance S, et al. Shoulder rotator
cuff disorders: a systematic review of clinical practice
guidelines and semantic analyses of recommendations.
Arch Phys Med Rehabil. 2020; 101 (7): 1233-1242. doi:
1016/j.apmr.2019.12.017.
Diercks R, Bron C, Dorrestijn O et al. Guideline for
diagnosis and treatment of subacromial pain syndrome:
a multidisciplinary review by the Dutch Orthopedic
Association. Acta Orthop. 2014; 85: 314-322. doi:
3109/17453674.2014.920991.
Longo UG, Risi Ambrogioni L, Berton A, et al. Physical
therapy and precision rehabilitation in shoulder rotator
cuff disease. Int Orthop. 2020; 44 (5): 893-903. doi:
1007/s00264-020-04511-2.
Macías-Hernández SI, García-Morales JR, Hernández-
Díaz C, Tapia-Ferrusco I, Velez-Gutiérrez OB, Nava-
Bringas TI. Tolerance and effectiveness of eccentric
vs. concentric muscle strengthening in rotator cuff
partial tears and moderate to severe shoulder pain. A
randomized pilot study. J Clin Orthop Trauma. 2020;
: 106-112. doi: 10.1016/j.jcot.2020.07.031.
Ladermann A, Burkhart SS, Hoffmeyer P, Neyton
L, Collin P, Yates E, Denard PJ. Classification of
full-thickness rotator cuff lesions: a review. EFORT
Open Rev. 2017; 1 (12): 420-430. doi: 10.1302/2058-
1.160005.
De la Rosa-Morillo F, Galloza-Otero JC, Micheo
W. Rehabilitacion del hombro doloroso en el atleta
joven [Shoulder pain rehabilitation in young athletes].
Rehabilitacion (Madr). 2019; 53 (2): 85-92. Spanish. doi:
1016/j.rh.2018.10.005.
Osborne JD, Gowda AL, Wiater B, Wiater JM.
Rotator cuff rehabilitation: current theories and
practice. PhysSportsmed. 2016; 44 (1): 85-92. doi:
1080/00913847.2016.1108883.
Schmidt CC, Jarrett CD, Brown BT. Management of
rotator cuff tears. J Hand Surg Am. 2015; 40 (2): 399-
doi: 10.1016/j.jhsa.2014.06.122.
Nikolaidou O, Migkou S, Karampalis C. Rehabilitation
after rotator cuff repair. Open Orthop J. 2017; 11: 154-
doi: 10.2174/1874325001711010154.
Gutman MJ, Joyce CD, Patel MS, et al. Early repair
of traumatic rotator cuff tears improves functional
outcomes. J Shoulder Elbow Surg. 2021; 30 (11): 2475-
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2023 Instituto Nacional de Rehabilitación Luis Guillermo Ibarra Ibarra

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.
© Instituto Nacional de Rehabilitación Luis Guillermo Ibarra Ibarra under a Creative Commons Attribution 4.0 International (CC BY 4.0) license which allows to reproduce and modify the content if appropiate recognition to the original source is given.