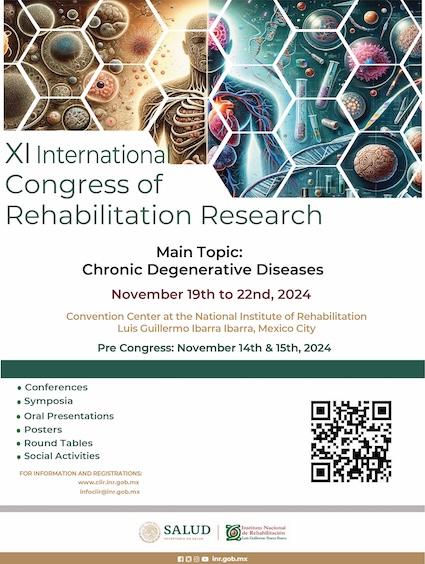
Sleep disorders in patients with acquired brain damage, associated factors and their impact on functionality
DOI:
https://doi.org/10.35366/103939Keywords:
Stroke, brain traumatic injury, sleep disorders, functionalityAbstract
Objective: To identify the prevalence of sleep disorders in chronic post-stroke and post-traumatic
brain injury (TBI) patients, to determine the risk factors and their impact on functionality in activities of daily life. Material and methods: Cross-sectional clinical study that included adults ≥ 18 years with a history of acquired brain damage (post-stroke or post-TBI). Sociodemographic data and clinical history were obtained, and the following instruments were applied: Pittsburgh Sleep Quality Index, the Epworth Sleepiness Scale, the Berlin Questionnaire© Sleep Apnea, the Barthel’s functionality index, the Hamilton Depression Rating Scale and the Beck Anxiety Inventory. Results: We included 116 patients, 91 post-stroke (78.4%) and 25 post-TBI (21.6%), mean age was 56.58 years (SD=19.37). In post-stroke patients, the following risk factors were identified: diabetes (OR=3.01; 95% CI=1.13-8.01 for poor sleep quality), multiple comorbidities (OR=3.78; 95% CI=1.04-13.67 for quality of sleep), depression (OR=2.46; 95% CI=2.46-25.80 for apnea; OR=7.94; 95% CI=1.25-10.82 for insomnia) and anxiety (OR=17.84; 95% CI=2.28-139.64 for insomnia). In post-TBI patients, the following were identified as risk factors: overweight/obesity (OR=11.25; 95% CI=1.64-76.84 for poor sleep quality) and coma (OR=2.33; 95% CI=1.42-3.82 for sleepiness). The risk factor for functional loss in post-stroke is apnea (OR=2.63; 95% CI=1.05-6.54) and in post-TBI the poor quality of sleep (OR=8.25; 95% CI=1.15-50.03). Conclusion: Post-stroke and post-TBI patients have a high prevalence of sleep disorders and its comorbidities increase the risk of chronic sleep disorders and functional loss.
References
Hermann DM, Bassetti CL. Sleeprelated breathing and
sleep-wake disturbances in ischemic stroke. Neurology.
; 73 (16): 1313-1322.
Hepburn M, Bollu PC, French B, Sahota P. Sleep
medicine: Stroke and sleep. Mo Med. 2018; 115 (6):
-532.
Ouellet MC, Beaulieu-Bonneau S, Morin CM. Insomnia
in patients with traumatic brain injury: frequency,
characteristics, and risk factors. J Head Trauma Rehabil.
; 21 (3): 199-212.
Crichton T, Singh R, Abosi-Appeadu K, Dennis G.
Excessive daytime sleepiness after traumatic brain injury.
Brain Inj. 2020; 34 (11): 1525-1531.
Viola-Saltzman M, Musleh C. Traumatic brain injuryinduced sleep disorders. Neuropsychiatr Dis Treat. 2016;
: 339-348.
Grima NA, Rajaratnam SMW, Mansfield D, SlettenTL,
Spitz G, Ponsford JL. Efficacy of melatonin for sleep
disturbance following traumatic brain injury: a randomised
controlled trial. BMC Med. 2018; 16 (1): 8.
Rundo JV, Downey R 3rd. Polysomnography. Handb
Clin Neurol. 2019; 160: 381-392.
Yi H, Shin K, Shin C. Development of the sleep quality
scale. J Sleep Res. 2006; 15 (3): 309-316.
Kaneko Y, Hajek VE, Zivanovic V, Raboud J, Bradley TD.
Relationship of sleep apnea to functional capacity and
length of hospitalization following stroke. Sleep. 2003;
(3): 293-297.
Winward C, Sackley C, Metha Z, Rothwell PM. A
population-based study of the prevalence of fatigue after
transient ischemic attack and minor stroke. Stroke. 2009;
(3): 757-761.
Muraki I, Wada H, Tanigawa T. Sleep apnea and type 2
diabetes. J Diabetes Investig. 2018; 9 (5): 991-997.
Hayashino Y, Yamazaki S, Nakayama T, Sokejima S,
Fukuhara S. Relationship between diabetes mellitus and
excessive sleepiness during driving. Exp Clin Endocrinol
Diabetes. 2008; 116 (1): 1-5.
Ogilvie RP, Patel SR. The epidemiology of sleep and
diabetes. Curr Diab Rep. 2018; 18 (10): 1-11.
Siarnik P, Klobucníková K, Surda P, Putala M, Sutovsky
S, Kollár B et al. Excessive daytime sleepiness in acute
ischemic stroke: Association with restless legs syndrome,
diabetes mellitus, obesity, and sleep-disordered
breathing. J Clin Sleep Med. 2018; 14 (1): 95-100.
Sutton EL. Psychiatric disorders and sleep issues. Med
Clin North Am. 2014; 98 (5): 1123-1143.
Blake MJ, Trinder JA, Allen NB. Mechanisms underlying
the association between insomnia, anxiety, and
depression in adolescence: Implications for behavioral
sleep interventions. Clin Psychol Rev. 2018; 63: 25-40.
Muscogiuri G, Barrea L, Annunziata G, Di Somma C,
Laudisio D, Colao A et al. Obesity and sleep disturbance:
the chicken or the egg? Crit Rev Food Sci Nutr. 2019;
(13): 2158-2165.
Ding C, Lim LL, Xu L, Kong APS. Sleep and obesity. J
obes metab syndr. 2018; 27 (1): 4.
Wolfe LF, Sahni AS, Attarian H. Sleep disorders in
traumatic brain injury. NeuroRehabilitation. 2018; 43 (3):
-266.
Grassi L, Kacmarek R, Berra L. Ventilatory mechanics in
the patient with obesity. Anesthesiology. 2020; 132 (5):
-1256.
Baumann CR, Werth E, Stocker R, Ludwig S, Bassetti
CL. Sleep-wake disturbances 6 months after traumatic
brain injury: a prospective study. Brain. 2007; 130 (7):
-1883.
Gilbert KS, Kark SM, Gehrman P, Bogdanova Y. Sleep
disturbances, TBI and PTSD: Implications for treatment
and recovery. Clin Psychol Rev. 2015; 40: 195-212
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Instituto Nacional de Rehabilitación Luis Guillermo Ibarra Ibarra

This work is licensed under a Creative Commons Attribution 4.0 International License.
© Instituto Nacional de Rehabilitación Luis Guillermo Ibarra Ibarra under a Creative Commons Attribution 4.0 International (CC BY 4.0) license which allows to reproduce and modify the content if appropiate recognition to the original source is given.