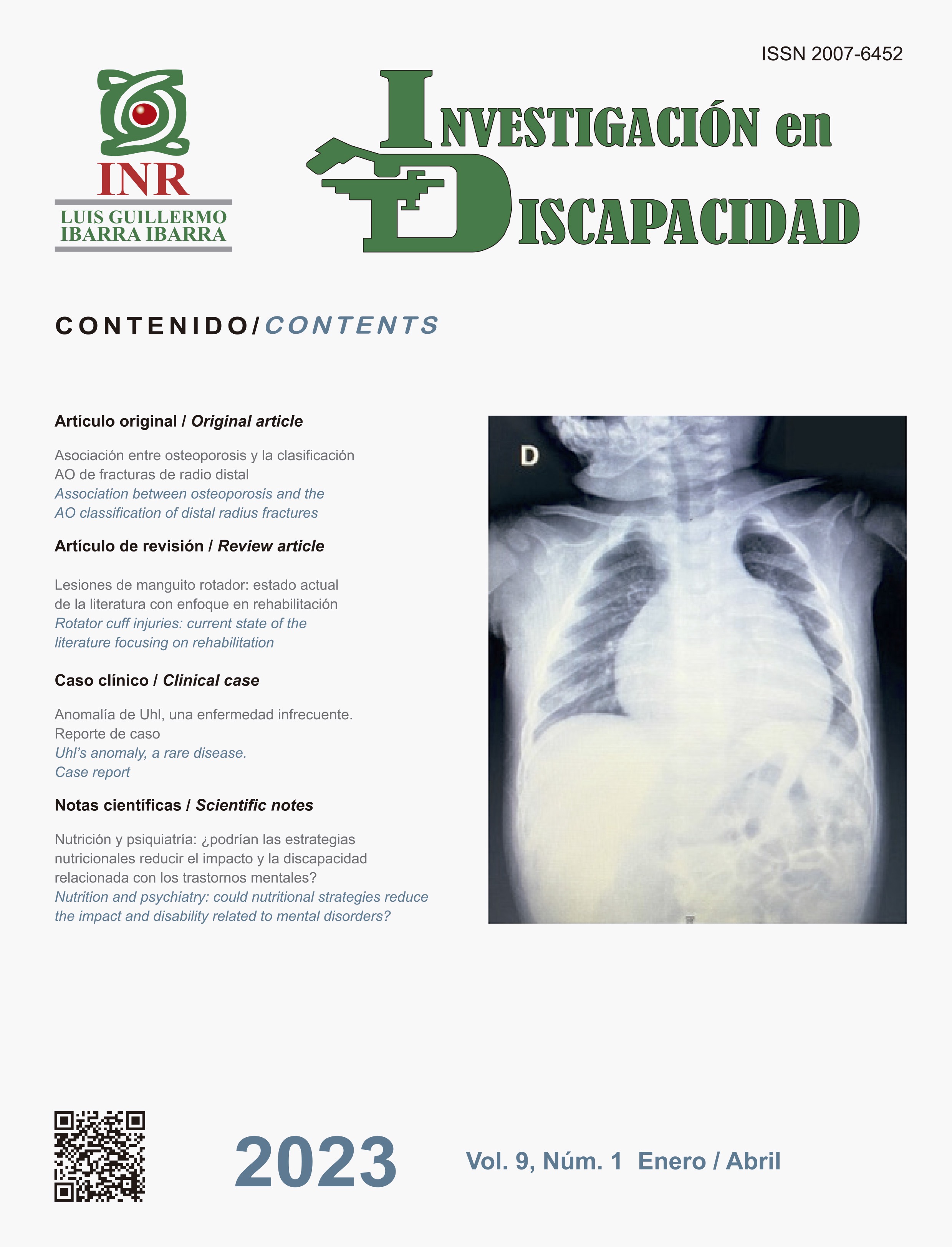
Association between osteoporosis and the AO classification of distal radius fractures
DOI:
https://doi.org/10.35366/109507Keywords:
bone density, densitometry,, osteoporosis, radius fracture, wristAbstract
Introduction: bone mineral density (BMD) is a known risk factor for distal radius fractures. However,
there is no reported evidence of the association between low BMD and the complexity of the fracture
line. Objective: this study attempts to find the association of low BMD, as well as other risk factors,
with the AO (Arbeitsgemeinschaft für Osteosynthesefragen) classification of distal radius fracture.
Material and methods: 144 medical records of patients older than 44 years of age with information
on centripetal bone mineral density, smoking habit, body mass index and mechanism of trauma
were studied. Fractures were classified according to the AO 2018 system using tomography with
3D reconstruction. Results: it was found that there is a relationship between a low BMD with simple
fracture lines if they were due to a low energy mechanism (OR = 0.15; p = 0.009). However, the
high energy mechanism increases the risk of suffering complex fractures regardless of the degree
of BMD (OR = 5.56). Conclusion: there is a relationship between a low BMD and a simple line of
distal radius fracture according to the AO classification. However, a high-energy trauma mechanism
is a sufficient factor to generate a complex fracture line.
References
Nellans KW, Kowalski E, Chung KC. The epidemiology of
distal radius fractures. Hand Clin. 2012 May;28(2):113-
doi: 10.1016/j.hcl.2012.02.001.
Azad A, Kang HP, Alluri RK, Vakhshori V, Kay HF,
Ghiassi A. Epidemiological and treatment trends of
distal radius fractures across multiple age groups. J
Wrist Surg. 2019; 8 (4): 305-311. doi: 10.1055/s-0039-
Porrino JA Jr, Maloney E, Scherer K, Mulcahy H, Ha
AS, Allan C. Fracture of the distal radius: epidemiology
and premanagement radiographic characterization. AJR
Am J Roentgenol. 2014; 203 (3): 551-559. doi: 10.2214/
AJR.13.12140
Stirling ERB, Johnson NA, Dias JJ. Epidemiology of
distal radius fractures in a geographically defined adult
population. J Hand Surg Eur. 2018; 43 (9): 974-982. doi:
1177/1753193418786378.
Kwan K, Lau TW, Leung F. Operative treatment of distal
radial fractures with locking plate system-a prospective
study. Int Orthop. 2011; 35 (3): 389-394. doi: 10.1007/
s00264-010-0974-z.
Levin LS, Rozell JC, Pulos N. Distal radius fractures in
the elderly. J Am Acad Orthop Surg. 2017; 25 (3): 179-
doi: 10.5435/JAAOS-D-15-00676.
Luokkala T, Laitinen MK, Hevonkorpi TP, Raittio L,
Mattila VM, Launonen AP. Distal radius fractures in
the elderly population. EFORT Open Rev. 2020; 5 (6):
-370. doi: 10.1302/2058-5241.5.190060.
NIH Consensus Development Panel on Osteoporosis
Prevention, Diagnosis, and Therapy, March 7-29, 2000:
highlights of the conference. South Med J. 2001; 94 (6):
-573.
World Health Organization. WHO Scientific Group
on the assessment of osteoporosis at primary health
care level: Summary meeting report; May5–7, 2004,
Brussels, Belgium. Geneva, Switzerland: World Health
Organization, 2007, 1-17.
Ostergaard PJ, Hall MJ, Rozental TD. Considerations
in the treatment of osteoporotic distal radius fractures
in elderly patients. Curr Rev Musculoskelet Med. 2019;
(1): 50-56. doi: 10.1007/s12178-019-09531-z.
Arora R, Gabl M, Erhart S, Schmidle G, Dallapozza
C, Lutz M. Aspects of current management of distal
radius fractures in the elderly individuals. Geriatr
Orthop Surg Rehabil. 2011; 2 (5-6): 187-194. doi:
1177/2151458511426874.
Ring D, Jupiter JB. Treatment of osteoporotic distal
radius fractures. Osteoporos Int. 2005; 16 Suppl 2:
S80-84. doi: 10.1007/s00198-004-1808-x.
Jupiter JB, Fernandez DL. Comparative classification
for fractures of the distal end of the radius. J Hand
Surg Am. 1997; 22 (4): 563-571. doi: 10.1016/S0363-
(97)80110-4.
Jayakumar P, Teunis T, Giménez BB, Verstreken
F, Di Mascio L, Jupiter JB. AO distal radius fracture
classification: global perspective on observer agreement.
J Wrist Surg. 2017; 6 (1): 46-53. doi: 10.1055/s-0036-
Graff S, Jupiter J. Fracture of the distal radius:
classification of treatment and indications for external
fixation. Injury. 1994; 25 Suppl 4: S-D14-25. doi:
1016/0020- 1383(95)90125-6.
Waever D, Madsen ML, Rolfing JHD, Borris LC,
Henriksen M, Nagel LL, Thorninger R. Distal radius
fractures are difficult to classify. Injury. 2018; 49 Suppl
: S29-S32. doi: 10.1016/S0020-1383(18)30299-7.
Yinjie Y, Gen W, Hongbo W, Chongqing X, Fan Z, Yanqi
F, Xuequn W, Wen M. A retrospective evaluation of
reliability and reproducibility of Arbeitsgemeinschaftfür
Osteosynthesefragen classification and Fernandez
classification for distal radius fracture. Medicine
(Baltimore). 2020; 99 (2): e18508. doi: 10.1097/
MD.0000000000018508.
Nogueira AF, Moratelli L, Martins MDS, Iupi RT, de
Abreu MFM, Nakamoto JC. Evaluation of distal forearm
fractures using the AO 2018 classification. Acta Ortop
Bras. 2019; 27 (4): 220-222. doi: 10.1590/1413-
Bain GI, MacLean SBM, McNaughton T, Williams R.
Microstructure of the distal radius and its relevance to
distal radius fractures. J Wrist Surg. 2017; 6 (4): 307-
doi: 10.1055/s-0037-1602849. Epub 2017 May 10.
Erratum in: J Wrist Surg. 2017; 6 (4): e1-e2.
Majumdar S, Genant HK, Grampp S, Newitt DC,
Truong VH, Lin JC, Mathur A. Correlation of trabecular
bone structure with age, bone mineral density, and
osteoporotic status: in vivo studies in the distal radius
using high resolution magnetic resonance imaging. J
Bone Miner Res. 1997; 12 (1): 111-118. doi: 10.1359/
jbmr.1997.12.1.111.
Daniels AM, Theelen LMA, Wyers CE, Janzing
HMJ, van Rietbergen B, Vranken L et al. Bone
microarchitecture and distal radius fracture pattern
complexity. J Orthop Res. 2019; 37 (8): 1690-1697.
doi: 10.1002/jor.24306.
Lill CA, Goldhahn J, Albrecht A, Eckstein F, Gatzka C,
Schneider E. Impact of bone density on distal radius
fracture patterns and comparison between five different
fracture classifications. J Orthop Trauma. 2003; 17 (4):
-278. doi: 10.1097/00005131- 200304000-00005.
Clayton RA, Gaston MS, Ralston SH, Court-Brown CM,
McQueen MM. Association between decreased bone
mineral density and severity of distal radial fractures.
J Bone Joint Surg Am. 2009; 91 (3): 613-619. doi:
2106/JBJS.H.00486.
De Klerk G, Han Hegeman J, Duis HJ. The relation
between AO-classification of distal radial fractures and
bone mineral density. Injury. 2013; 44 (11): 1657-1658.
doi: 10.1016/j.injury.2013.02.007.
Dhainaut A, Daibes K, Odinsson A, Hoff M, Syversen U,
Haugeberg G. Exploring the relationship between bone
density and severity of distal radius fragility fracture in
women. J Orthop Surg Res. 2014; 9: 57. doi: 10.1186/
s13018-014-0057-8.
Hjelle AM, Gjertsen JE, Apalset EM, Nilsen RM, Lober A,
Tell GS et al. No association between osteoporosis and
AO classification of distal radius fractures: an observational
study of 289 patients. BMC Musculoskelet Disord. 2020;
(1): 811. doi: 10.1186/s12891-020-03842-w.
Obert L, Loisel F, Jardin E, Gasse N, Lepage D. High-energy
injuries of the wrist. Orthop Traumatol Surg Res. 2016; 102
(1 Suppl): S81-93. doi: 10.1016/j.otsr.2015.05.009.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Instituto Nacional de Rehabilitación Luis Guillermo Ibarra Ibarra

This work is licensed under a Creative Commons Attribution 4.0 International License.
© Instituto Nacional de Rehabilitación Luis Guillermo Ibarra Ibarra under a Creative Commons Attribution 4.0 International (CC BY 4.0) license which allows to reproduce and modify the content if appropiate recognition to the original source is given.